Materials & methods: customized titanium lattice structure...
Materials and Methods
Participant
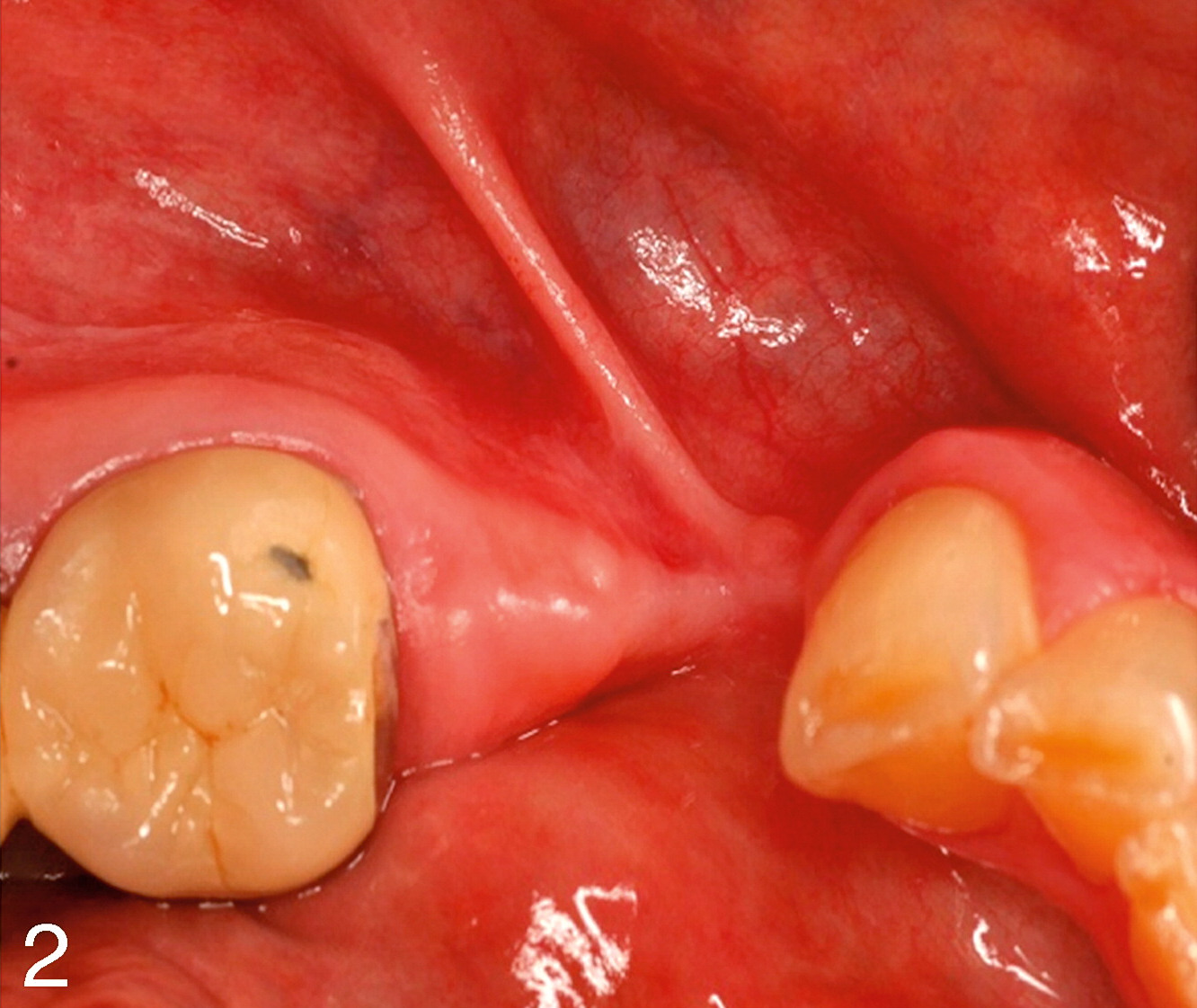
A 61-year-old healthy woman without any medical history showed a highly atrophied segment of the right lower posterior mandible (#29 and #28). The significant vertical and transversal deficit, as well as the challenging soft tissue situation, made a functionally and esthetically satisfying implant placement impossible (Figures 1 and 2).

Design and material
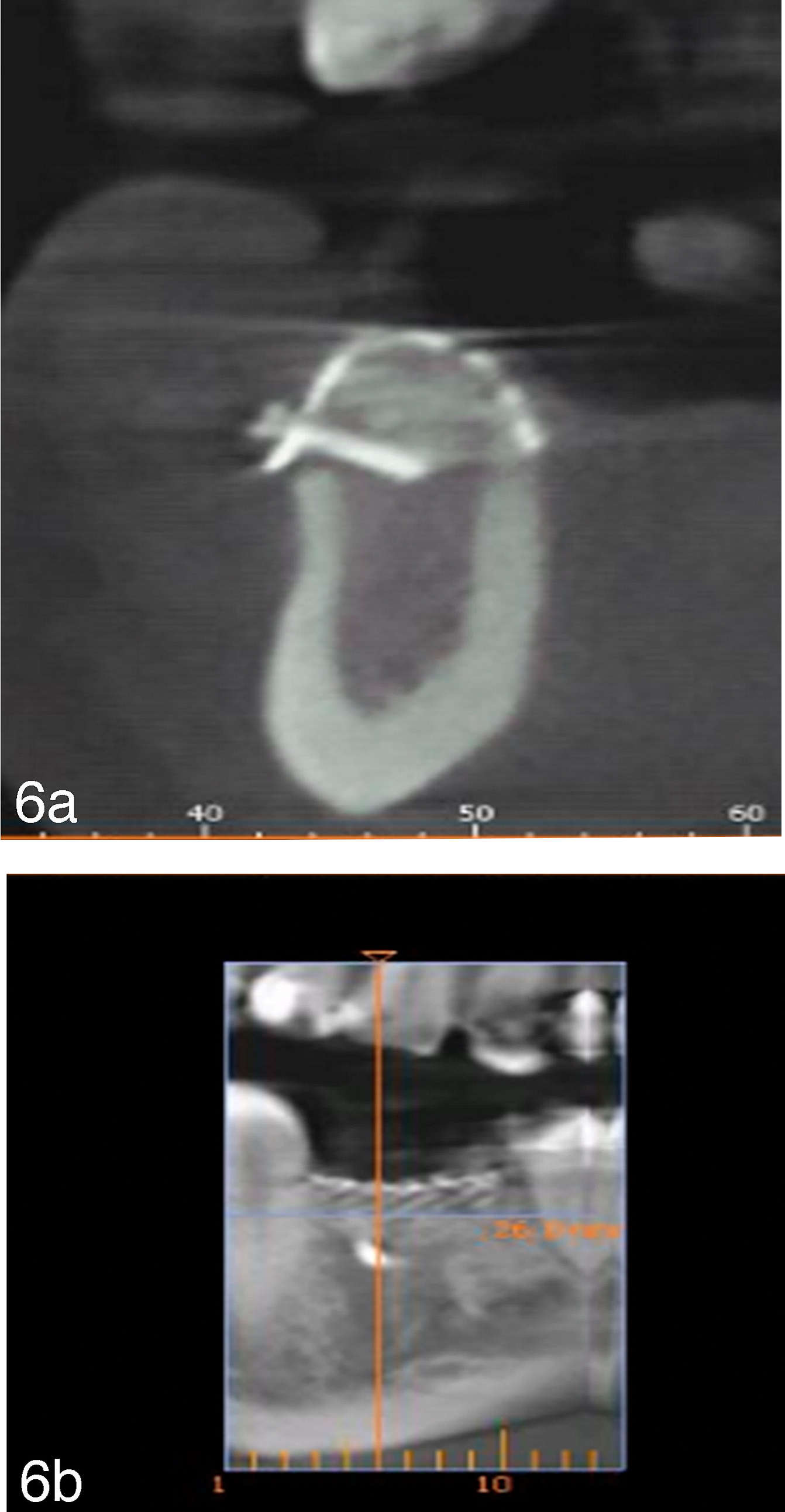
After clinical examination of oral hard and soft tissue, radiographic analysis was performed. After the acquisition of cone beam computerized tomography (CBCT) data, the three-dimensional model of the bony defect proved to be an inadequate bony situation for implant placement. Augmentation procedure was planned by using a prefabricated titanium lattice structure (Yxoss CBR, ReOss, Filderstadt, Germany) and graft material. Comprehensive information about the individualized lattice structure, xenogenic allograft, and surgery were provided, and informed consent was obtained. Treatment alternatives such as removable prothesis were declined by the patient.
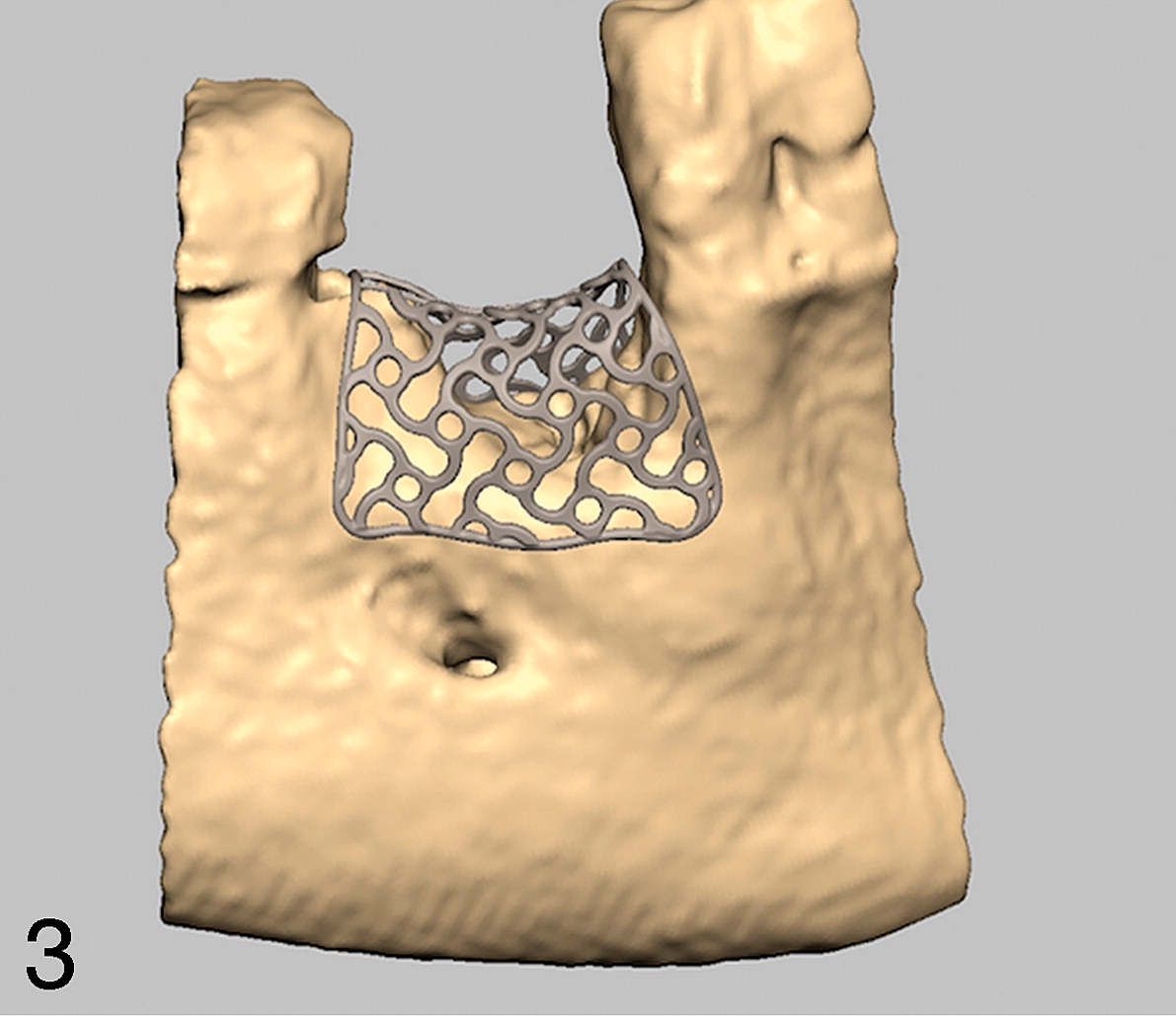
The patient-specific lattice structure was designed using computer-aided design/computer-aided manufacturing (CAD/CAM) technology by generating a three-dimensional model of the bony defect after CBCT with minimum artifacts from conventional digital imaging and communication in medicine (DICOM) files. The scan data were transferred and modified by reverse engineering software. The individualized lattice structure was designed according to the desired augmentation volume in the envelope (Figure 3). The final design was approved digitally by the surgeon and then manufactured. Costs depend on size of the defect and subsequent size of the lattice structure.
Procedure
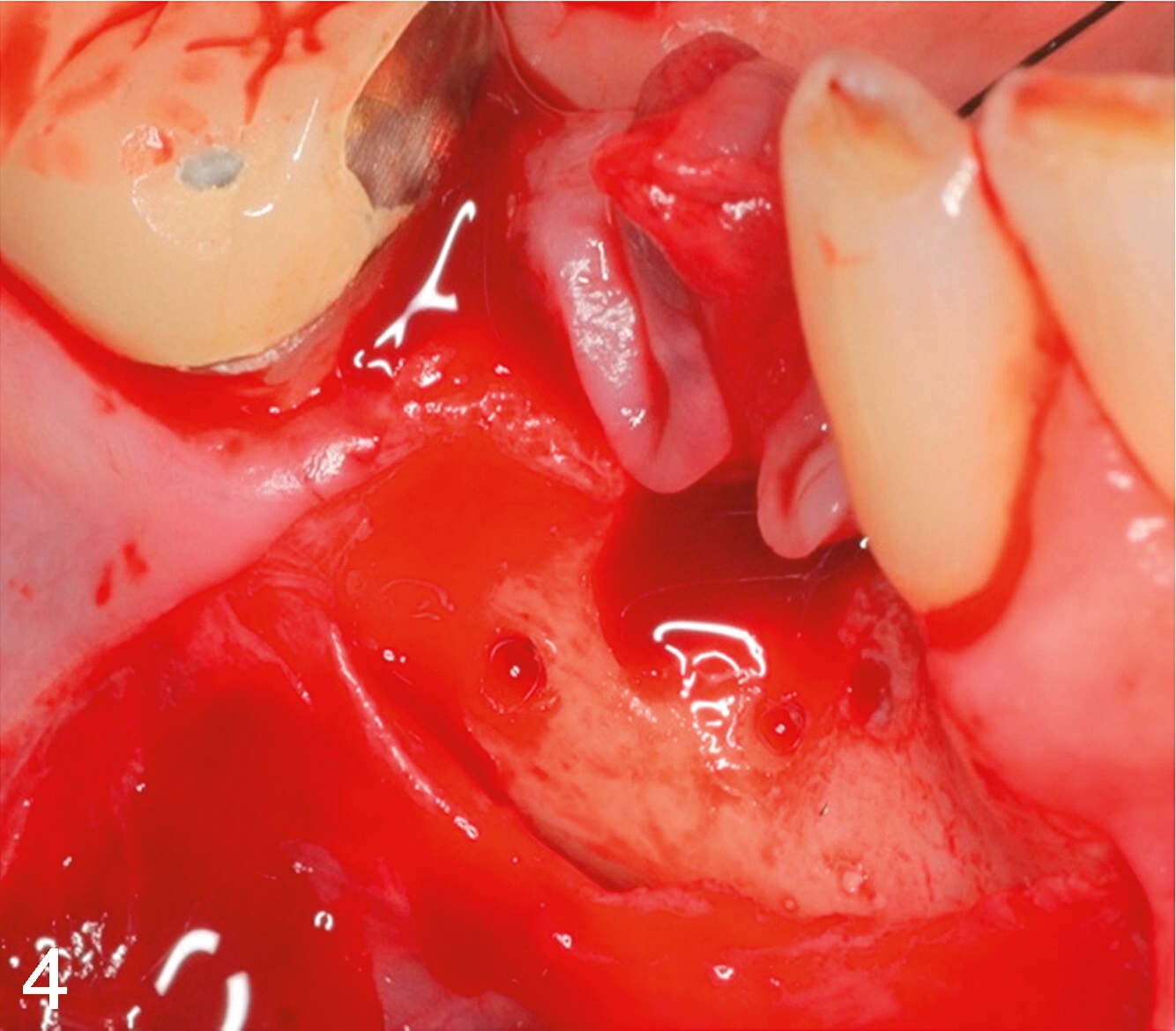
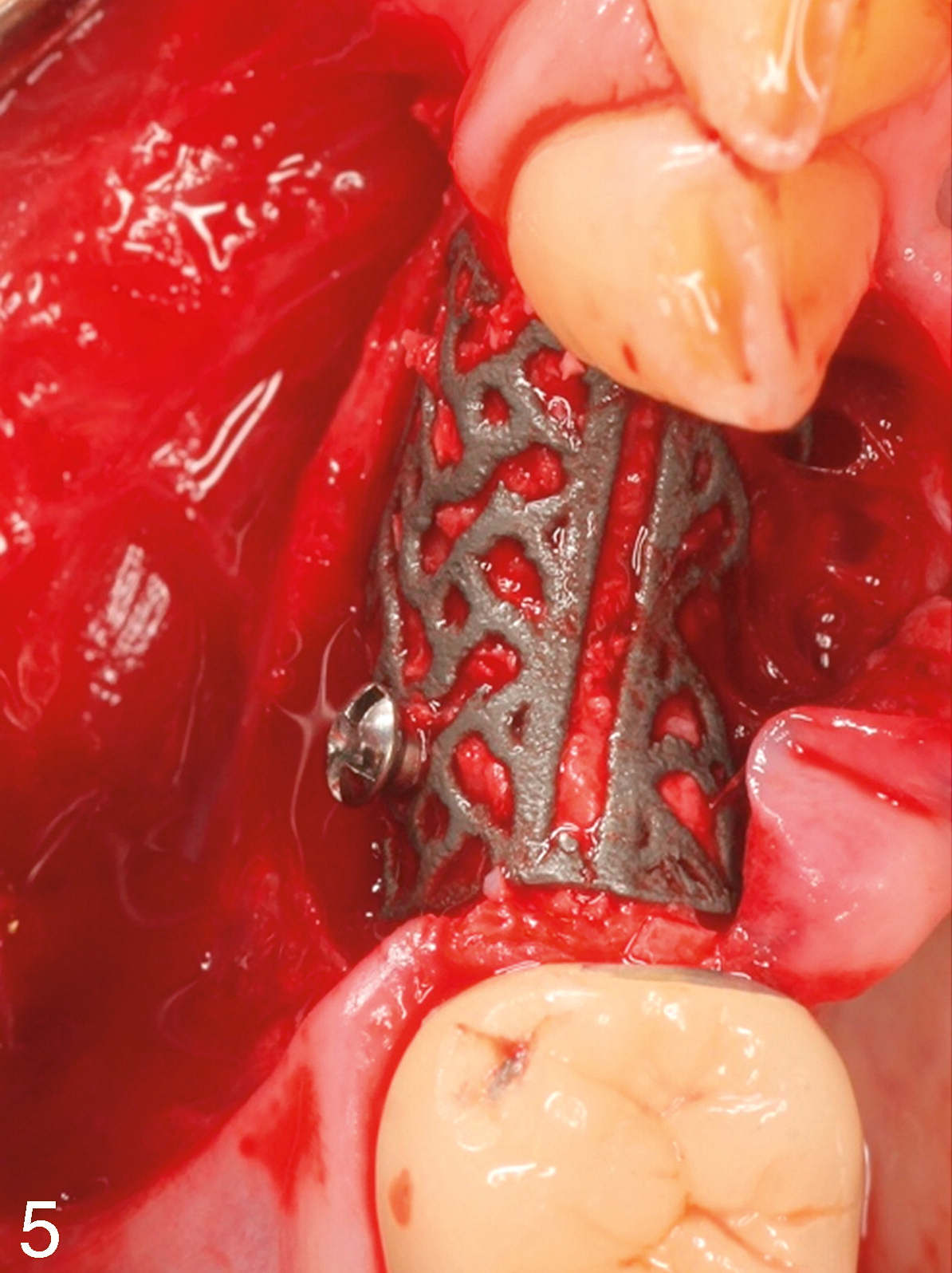
Surgery was performed under local anesthesia (Ultracain DS Forte, Ultracain, Hoechst, Germany). After elevation of a marginal soft tissue split flap starting in the vestibular gingival mucosa (about 12 – 15 mm vestibular from the mucogingival junction), scar tissue was removed, and the defect was visualized (Figure 4). The prefabricated titanium lattice structure was inserted with a passive tension-free fit keeping the biological precautions (1.5 mm to the adjacent teeth or nerve structures). Graft material from local bone obtained from the ramus of the mandible was mixed with xenogenic alloplastic material (Bio Oss, Geistlich Pharma, Wolhusen, Switzerland) in a ratio 1:1. Stable fixation of the lattice structure on the residual local bone was achieved by use of one osteosynthesis screw (Ø 2 mm/9 mm, Medicon eG, Tuttlingen, Germany) (Figure 5). Wound closure was achieved by suturing without tension. Postoperative instructions such as avoidance of the prosthesis were given to the patient, as well as detailed instructions about oral hygiene.



At suture removal (day 10) and during wound healing, a clinically healthy marginal area and full soft tissue coverage of the customized titanium lattice structure were present.
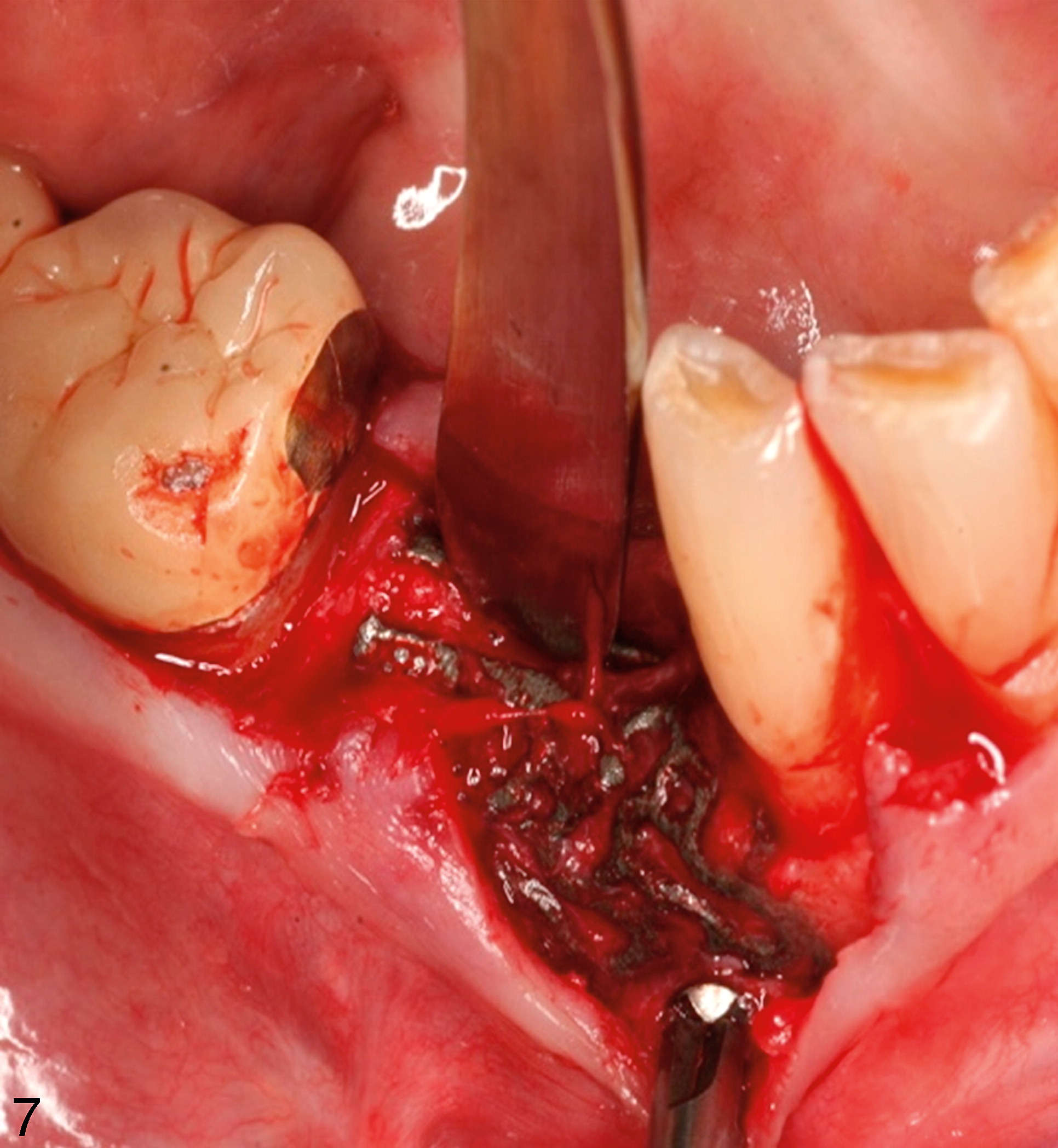
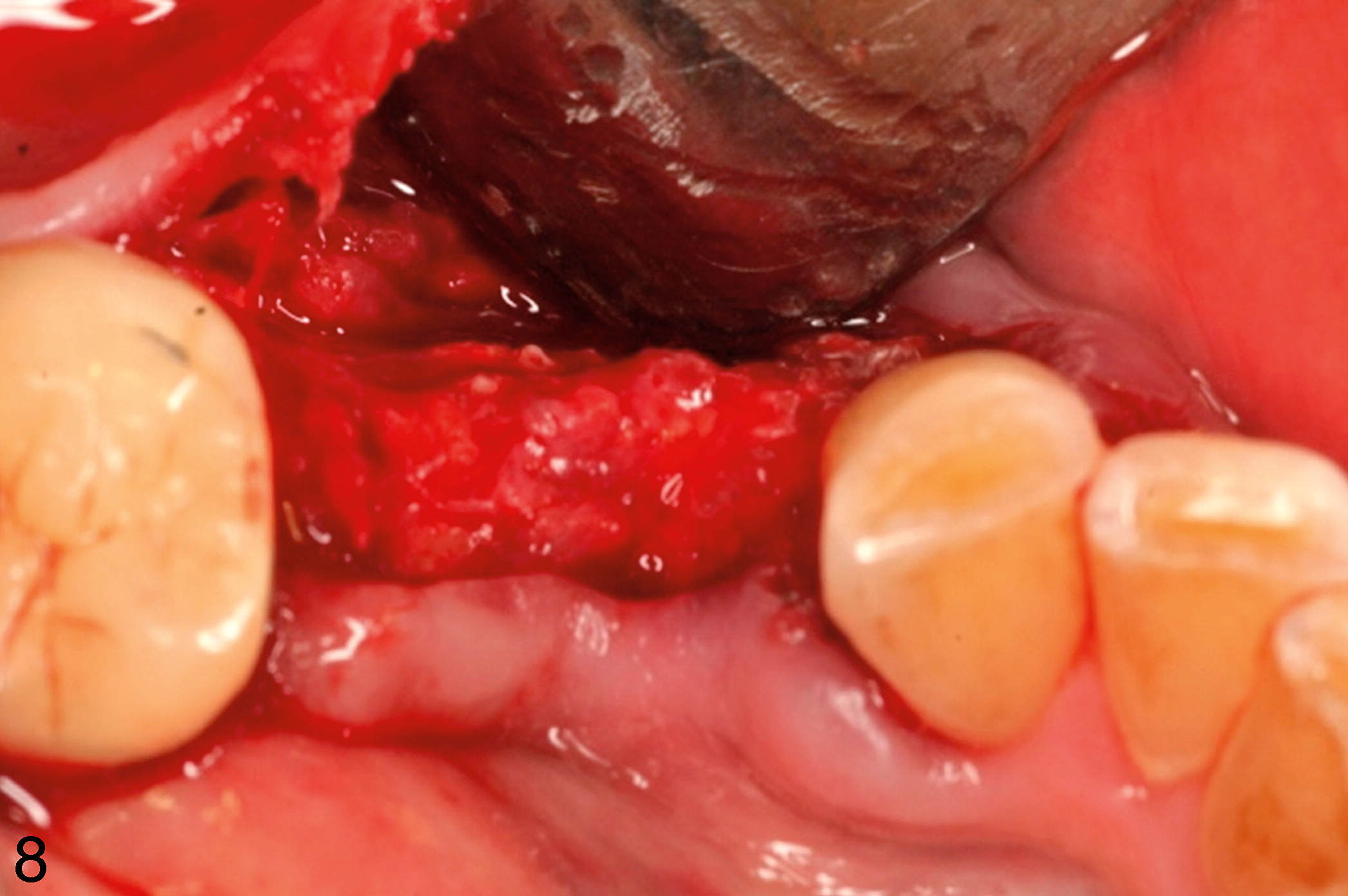
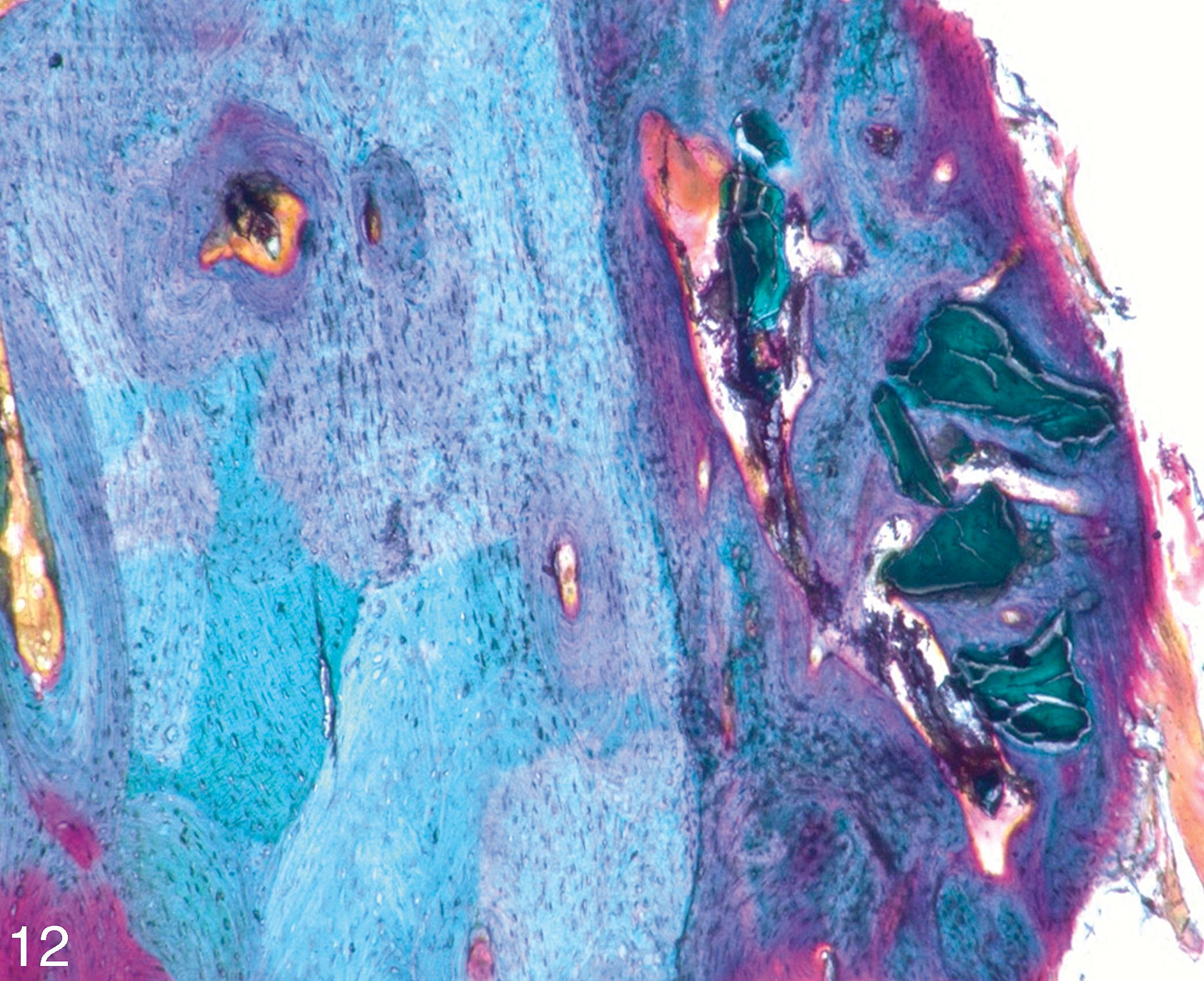
After a healing period of 6 months, a new CBCT dataset was collected to verify enhancement of the bone augmentation volume (Figure 6) and to plan implant surgery and removal of the lattice structure. For this second surgery, the same local anesthesia was used. After preparation of a mucoperiosteal full-thickness flap, the fixation screw was removed. By applying rotating focus with an elevator at the predetermined breaking point (Easy Removal Design, ReOss) the lattice structure is divided in two parts (Figure 7). The augmented bone volume was of stable dimension, well-vascularized, and without any signs of inflammation (Figure 8). The implant placement was performed following the standard procedures, and a cylindrical bone specimen was gained followed by a tension-free wound closure. The sutures were removed 1 week later.
The implants were functionally loaded after 4 months using a hybrid bridge according to the patient's wishes and preferred concept of the referral practice.
Serial posts:
- Customized Titanium Lattice Structure in Three-Dimensional Alveolar Defect: An Initial Case Letter
- Introduction: customized titanium lattice structure...
- Materials & methods: customized titanium lattice structure...
- Result: customized titanium lattice structure...
- Discussion: customized titanium lattice structure...
- Conclusion: customized titanium lattice structure...
- Abbreviations: customized titanium lattice structure...
- Acknowledgments: customized titanium lattice structure...
- References: customized titanium lattice structure...