Case report: combination syndrome
Case Report
A 76-year-old woman with Sjogren syndrome presented complaining of a poor fit of an upper denture and difficulty chewing and speaking clearly. Patient had Sjogren syndrome for the previous 20 years in a mild and controlled form. She had been using water to compensate for dryness of her mouth and was taking prednisone 10 mg every other day for the last 2 years. Otherwise, patient's medical history was not contributory.
The patient lost some of her upper front teeth about 50 years ago and had a bridge, but eventually lost her remaining upper front teeth requiring a partial denture. She has had 2 sets of dentures for her upper jaw for the past 15 years with the second one constructed less than a year prior to her implant consultation. Patient was wearing a removable maxillary partial denture retained by the bridge No. 12-13-14 on the left side and tooth No. 2 on the right. Due to recent mobility of her upper right second molar (No. 2), her new partial denture became loose and difficult to wear. She had a previous experience with a blade implant for her lower jaw, was satisfied with it and now was interested in exploring an implant treatment for her upper jaw.
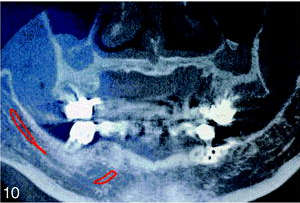
On examination, the patient presented with the maxillary RPD for the anterior edentulous area crossing the midline and bounded by the presence of posterior molars, severe maxillary bone deficiency especially in the premaxillary area, and prognathic appearing mandible (pseudo class III jaw relationship). The anterior maxillary alveolar process was thin and deficient three-dimensionally with mobile hypertrophic tissue in place of the anterior alveolar crest and papillary hyperplasia of the hard palate's mucosa (Figure 6). The patient had 4 remaining upper posterior teeth: No. 2 (mobility three plus) and No. 12, No. 13, and No. 14 (stable with recently placed crowns connected in the bridge). The crown No. 2 and the bridge No. 12-13-14 had O-ring attachments on the mesial end of both restorations for retention of patient's upper partial denture (Figure 7). In the lower jaw, the patient had an old (20 years) well-integrated blade implant in the left premolar-molar region with an extension for No. 20 crown connected rigidly to the natural crown No. 22 (Figure 8). A moderate degree of extrusion of the lower anterior teeth was evident. Teeth No. 23 through 27 had short clinical porcelain fused to metal (PFM) crowns and were stable. The bridge No. 28-29-30 was in a poor periodontal state and temporarily was not included in the treatment plan per patient's request. To better assess premaxillary bone resorption, a tomographic three-dimensional bone survey (CT scan) was ordered. It demonstrated an advanced volumetric maxillary bone atrophy of the anterior maxilla, extending from No. 3 area on the right to tooth No. 12 on the left (Figures 9 and 10).



Serial posts:
- Combination Syndrome: Classification and Case Report
- Introduction: Combination Syndrome
- Case report: combination syndrome
- Diagnosis: Combination Syndrome
- Treatment Plan : Combination Syndrome
- Operative phase : Combination Syndrome
- Restorative stage : Combination Syndrome
- Classification : Combination Syndrome
- Discussion : Combination Syndrome
- Conclusion : Combination Syndrome
- References : Combination Syndrome
- Table Classification of combination syndrome (CS)
- Extended table of classification of Combination Syndrome (CS)